Why do I need a sleep study?
What are the Symptoms?
Do you have these symptoms?
- Need an alarm to wake up in the morning
- Snoring, choking, or gasping during sleep, or bed partner observes cessation of breathing
- Kicking your bed partner
- Restless legs sensation at sleep time
- Inability to initiate or maintain sleep that is negatively impacting your waking hours
- Dependent upon caffeine or other stimulants to get you through the day
If you do, you may be experiencing the result of poor quality sleep or fewer hours of sleep than you need. You may be struggling to do everyday tasks, be less alert, and you be more prone to accidents. Ask and listen to those around you about your sleep and productivity, write down your symptoms and chat with your doctor!
What are the Risks?
Our sleep can affect how long we live (1) and how well we live because poor sleep has been linked to high blood pressure, heart problems, stroke, diabetes, and obesity. If you regularly sleep less that 6-7 hours per night and you have the symptoms of poor sleep, you are at risk for accidents and injury to ourselves and others. In addition, in the long term, you are at risk for memory loss and decreased productivity. Sleep must be made a priority to reduce the risks of injury to ourselves and others.
One of the most life threadtening of sleep disorders is obstructive sleep apnea.
What should I do?
- Talk to your doctor. Make a list of your sleep symptoms, be honest about how many hours you average a week, and include your friend and family’s observations in your list. Take this list with you when you visit your doctor who will make recommendations for next steps.
- Sleep Hygiene
-To pave the way for better sleep, follow these simple yet effective healthy sleep tips, including:- Stick to a sleep schedule, even on weekends.
- Practice a relaxing bedtime ritual.
- Exercise daily.
- Evaluate your bedroom to ensure ideal temperature, sound and light.
- Sleep on a comfortable mattress and pillows.
- Beware of hidden sleep stealers, like alcohol and caffeine.
- Turn off electronics before bed.
- Sleep Study – Sleep studies help doctors diagnose sleep abnormalities such as sleep apnea (cessation of breathing during sleep), movement disorders such as uncontrollable leg jerks, and other disorders that may cause medical problems and/or daytime sleepiness. For Kaiser Hawaii patients, sleep studies may be done either in a sleep laboratory where you spend the night (or day if you are a shift worker) or in your home. Regardless of location, the sleep study requires sensors that are temporarily attached to the skin and scalp (in-lab only). Sleep studies are not typically used for sleep disruption caused by Circadian Rhythm (Body Clock) Disorders such as jet lab or shiftwork.

Next Step: Sleep Study
Sleep studies are tests that record what you brain and body are doing during sleep. If sleep apnea is suspected, your heart, breathing, and oxygen level are recorded. If abnormal body movements or you are unable to fall asleep or stay asleep, polysomnography, a sleep study that records brain and muscle activity to identify specific sleep stages, eye, and muscles activity may be done.
Where will you be tested?
You may be scheduled for either an In-Laboratory sleep study, or a Home Sleep Study.
- Home Sleep Studies are used for the diagnosis of obstructive sleep apnea (OSA) in patients who have a high probability of moderate to severe OSA or not possible to come into the lab (immobility, safety, or critical illness)
- In-Lab Sleep Studies are used for diagnosing sleep disorders such as periodic limb movements during sleep, and studies that require monitoring by a sleep technologist to adjust oxygen and therapeutic devices.
Below is a description of the two types of sleep study.
In-Lab Sleep Study

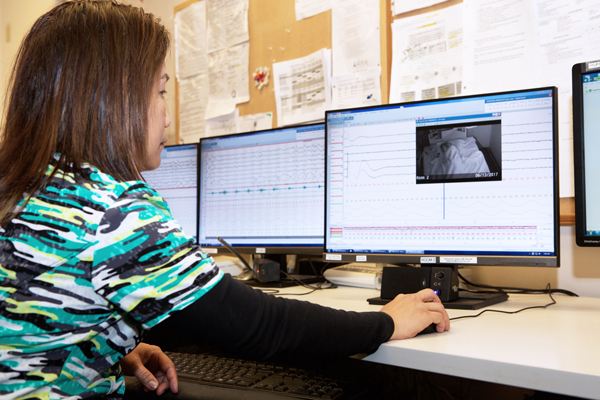
Once in the lab, you’ll be given pre-test instructions and on the night of the test, sleep technologists will provide instructions, apply sensors using tape (and paste for polysomnography tests), and monitor you while you sleep from the control room, as you sleep in a private room. The sleep rooms have a locker for your personal items (please leave valuables at home). A low-light camera allow the technologists to observe if you are sleeping on your side, back, or prone. An audio system allows the technologist to document snoring and hear you when you call during the night. The sensors can be quickly disconnected so you can go to the restroom as needed.
In the morning, the electrodes are removed, you can shower and go to work or pursue your regular activities. The sleep information that is collected is interpreted by a board certified sleep medicine physician. You should make a follow-up appointment with your doctor 3 weeks after the sleep study.
Discuss with your doctor any concerns you might have about not being able to sleep in a different environment. If you have special needs, please inform the Sleep Lab staff when they call to schedule and confirm your appointment.
Your sleep study may be done at either Oahu, Maui, or the Big Island. You may be referred to either the Kaiser Sleep Lab at the Moanalua Medical Center, in the Malama Ohana Wing, 1st Floor, or Kaiser Hawaii’s outsource labs on Oahu, Maui, or the Big Island.
Home Sleep Study

If your doctor refers you for home sleep apnea testing (HST), you will set up the testing equipment yourself and use the sleep monitor device in your own home. This allows collection of information about how you breathe during sleep.
You’ll be contacted to schedule you to attend a class with other Kaiser members and learn to use the home sleep apnea testing device that records your heart, breathing, and oxygen level. You’ll be shown how to attach the two sensors at bedtime and turn on the device. The next morning, you can remove the sensors and put it all back into the travel tote. You’ll have an appointment for this day so you can return the sleep device to the Sleep Lab and receive your preliminary sleep study results in 20 minutes.
If you have OSA, the sleep technologist will offer the option to schedule a home OSA treatment study, known as an Auto Positive Airway Pressure (APAP) Titration study.
Your recent ambulatory sleep study showed that you have sleep apnea. Sleep apnea occurs when tissue and muscles in the back of the throat and airway relax or collapse during sleep. This can stop the flow of air and oxygen the lungs and body. People with sleep apnea may stop breathing hundreds of times per night. Sleep apnea can lead to health problems such as high blood pressure, heart damage, heart attack, and stroke.
Auto Positive Airway Pressure (APAP) APAP is the most common and effective treatment for sleep apnea. The CPAP machine delivers a flow of positive pressure air through a mask to splint the airway open during sleep.
Auto CPAP Trial To determine your airflow treatment pressure, you will be fitted with a PAP mask which connects to an auto PAP machine. The auto PAP machine automatically adjusts the airflow pressure during the night to stop or decrease the apneas. . , The auto PAP machine will be on loan to you for a trial period of about 10 to 14 days. Most people learn to sleep with a APAP mask after an adjustment period. It’s important to work closely with the respiratory therapist who set you up with the APAP device to find the best fitting mask and accessories.
CPAP Treatment After the auto PAP trial period, your physician will discuss with you the results of your study and may prescribe a APAP mask, APAP machine, and airflow pressure for your nightly use.
What can be diagnosed?
The sleep study can diagnose: Sleep Disorders
- Sleep-related Breathing Disorders such as sleep apnea Has anyone ever told you that you seem to stop breathing when you sleep? Do you snore loudly and wake yourself up? Do you have morning headaches or sometimes feel like you are more tired when you wake up than when you went to bed? You may have sleep apnea. Apnea is cessation of breathing. You have sleep apnea when you stop breathing for 10 seconds or longer, 5 or more times per hour of sleep. The most common type of sleep apnea is obstructive sleep apnea (OSA), caused by either a decreased airway size due to tongue or soft tissues obstruction that worsens when we lie down. The body tries to breath and air cannot be inhaled to the lungs for needed oxygen and carbon dioxide gas exchange. The sensation can be that of choking or suffocation. You may be not be aware of this at all during the early years of OSA. OSA affects an estimated 42 million people in the U.S. and is increasing!
Who has OSA?
- 15-20% of men, 5-15% of women (1 in 4 women older than 65 have OSA)
- 1 in 5 adults have mild OSA
- 1 in 15 adults have moderate to severe OSA
- 70-80% of patients are undiagnosed!
- Sleep disrupting disorders such as Sleep Related Movement Disorders
- Restless Legs Syndrome (RLS) and Sleep
- Periodic Limb Movements in Sleep Periodic limb movements typically silent. You may have episodes of simple, repetitive muscle movements, commonly in the legs, but may be any extremity of the body. The jerks occur when tightening or flexing of an extremity muscle occurs and this may disrupt your sleep, or that of your partner, during the night. Typically you feel tired during the day.
- Teeth Grinding
(1) ©2017 National Sleep Foundation. All rights reserved. https://sleepfoundation.org/how-sleep-works/how-much-sleep-do-we-really-need